Gary's story
Gary Bethel, a 41-year old native of the Bahamas, led a relatively normal island life. He worked a full-time job alongside his father, loved spending time with family and enjoyed boating and fishing. Things changed for Gary one October day when he began to feel dizzy, short of breath and started to experience hallucinations. He knew something was wrong, so he headed to the local hospital where he was diagnosed with COVID-19, pneumonia, acute respiratory distress and acute kidney injury. His condition required more specialized medical attention than the hospital could provide, so he was transported by air to Kendall Regional Medical Center in Miami.
Once in Miami, Gary was given a tracheostomy and placed on a ventilator. He spent the next four weeks in a medically induced coma. When he awoke, Gary was confused and disoriented. It took him a few days to understand and come to terms with what happened to him. He was extremely weak from being bed-bound for so long, unable to do anything independently. Once Gary stabilized, his physicians recommended he continue with the next step of his recovery at West Gables Rehabilitation Hospital.
Upon arrival at West Gables, Gary was just beginning to orient himself to his new circumstances and surroundings. He was unable to walk, speak, ingest food and water, or move in his bed without assistance. Gary also needed help to complete any of his personal care needs. Making matters even more challenging, he experienced extreme fatigue which initially prevented him from making progress.
Gary’s first goal was to discontinue use of the ventilator. Respiratory therapists assessed Gary’s needs and immediately created a plan to liberate from the machine. They began to gradually reduce the air support he was receiving from the ventilator while closely monitoring his oxygen saturation and breathing quality. When Gary showed that he was able to breathe more independently with less support, respiratory therapists transitioned him to a tracheostomy collar, a medical device that secures a trach tube in position, allowing the patient to move more easily.
In time, Gary fully liberated and was placed on supplemental oxygen. He celebrated this achievement as a key turning point in his recovery and immediately set the next goal of completely weaning off of the supplemental oxygen. Within the first week off the ventilator, he was already requiring significantly less liters of oxygen flow; soon after, he required none at all and he was able to breathe on his own.
Gary’s occupational therapy team got right to work rebuilding his strength and endurance so he could begin to work on completing personal care activities more independently. Additionally, therapists used various activities to focus on improving functional mobility and making it easier for Gary to transfer in and out of bed with the help of assistive devices. Throughout his recovery, Gary learned energy conservation techniques so he could complete tasks despite his ongoing fatigue. Occupational therapists introduced a variety of activities to Gary to help him reach his goals, including boxing in therapy sessions.
In physical therapy, Gary and his therapists focused on improving strength, endurance and managing fatigue. Additionally, they focused on developing proper body mechanics to reduce straining joints and muscles and ensure safe movements. Gary practiced standing and walking, at times maneuvering around obstacles to fine-tune his balance. During the sessions, therapists would gradually reduce the frequency and duration of Gary’s breaks to help him build up endurance. They also encouraged Gary to complete exercises on his own between therapy sessions. Gary began walking longer distances without any breaks and was soon able to get out of bed without assistance and use a walker to walk independently.
Meanwhile, speech therapists worked with Gary to address his dysphagia, or difficulty swallowing, and to increase the amount of words he could speak per breath. They also taught him deep breathing exercises and swallowing strategies to avoid choking. As Gary progressed, he was able to eat more solid foods and drink thinner liquids by mouth. He worked tirelessly to improve his vocal quality so he could speak and be easily understood again.
Throughout his rehabilitation, Gary’s mother was his key supporter. She flew to Miami to accompany Gary on the first day of his hospitalization, stating that she would not travel back to the Bahamas until her son was well enough to travel back home with her. Gary’s mother did not miss a beat during Gary’s recovery journey, spending most days at the hospital and covering the walls of his room with family photos and inspirational quotes to help keep his spirits up. The rest of Gary’s family was also extremely supportive and spoke to him regularly through phone calls and video chats.
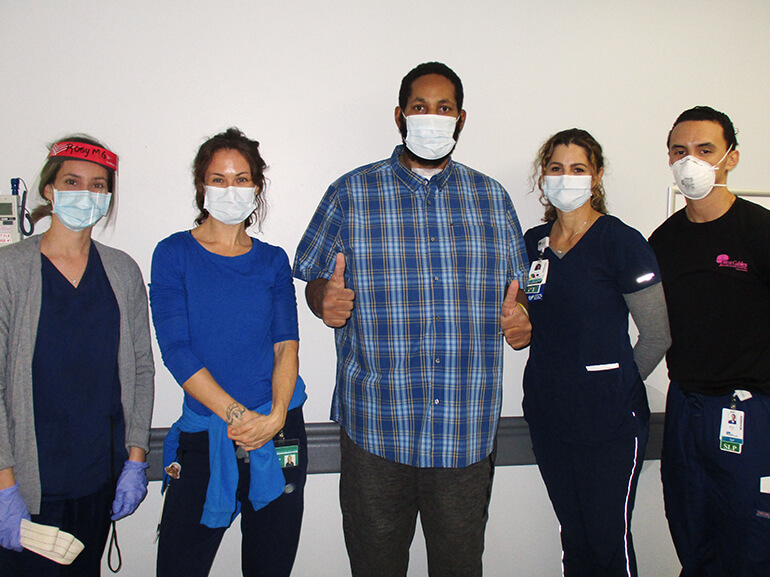
After nearly three weeks at West Gables Rehabilitation Hospital, Gary was strong enough to be discharged. He stated that he was excited to return home to the Bahamas so he could spend time with family and go out on his boat again. Gary has high praise for his experience at West Gables, saying, “Everything was great.” He further noted that he was especially pleased with his therapists and all the progress he made towards his goals.
Gary explained that his experience with COVID-19 and his subsequent recovery gave him the opportunity to reflect on life and realize what is truly important. “I gained a new strength that I did not know I possessed before,” Gary said. He also credits God and his faith for helping to get through these difficult times. Through all the challenges he faced, Gary maintained a positive attitude and never lost his sense of motivation. After having COVID-19 nearly take his life, Gary wants to urge others to take the proper precautions against the virus by getting vaccinated and following health guidelines.